The incidence rate of colorectal cancer has a rising trend in Hong Kong. According to the report from Hong Kong Cancer Registry (Hospital Authority), the incidence rate of colorectal cancer has risen from 4,335 to 5,635 in the year between 2009 and 2017. The report also stated that colorectal cancer is with the top most incidence rate among all cancers and its mortality rate is over 2,000 cases in the year 2017, which is just one place below the top most mortality cancer – lung cancer. With the rising number of incidence rate, we believe its mortality rate will soon exceed the death toll of lung cancer.
Although the actual cause of bowel cancer is still uncertain, medical professionals agree that the following populations belong to the high risk groups:
- Male
- Aged 50 or above
- Any first degree relatives with a history of bowel cancer (First degree relatives refer to parents, siblings, sons and daughters.)
Gastroenterologists have also conducted studies on bowel cancer from different perspectives; they found the followings may increase the risk of suffering from bowel cancer:
- History of colonic polyps or bowel cancer
- Suffered from Hereditary Non-polyposis Bowel cancer (HNPCC)
- Suffered from familial adenomatous polyposis (FAP)
- Suffered from Inflammatory Bowel Disease (IBD), including both patients of Crohn’s Disease and Ulcerative Colitis
- Daily diet rich in animal fat, protein and lacking dietary fiber
- Intake of large amount of red meat (e.g. Pork, beef and lamb) or processed meat
- Obesity, lack of sport, smoking or being alcoholic

As the clinical manifestations of bowel cancer are similar to that of common intestinal diseases, patients are prone to neglect the disease. Once diagnosed, it is usually at an advanced stage and the best timing for treatment is gone. American Cancer Society suggests that patients should immediate go to seek medical advices if any of the following sign or symptom is found:As the clinical manifestations of bowel cancer are similar to that of common intestinal diseases, patients are prone to neglect the disease. Once diagnosed, it is usually at an advanced stage and the best timing for treatment is gone. American Cancer Society suggests that patients should immediate go to seek medical advices if any of the following sign or symptom is found:
- Dark stools, rectal bleeding or blood in the stools
- Change of bowel habits, for example, constipation or diarrhea with unknown cause and lasting for several days
- Narrowing of stool
- Tenesmus (A feeling of incomplete defecation)
- Loss of appetite and weight with unknown cause
- Abdominal pain, distension or tangible mass with unknown cause
- Fatigue with unknown cause
In addition, bowel cancer is not an acute disease; it takes long time to develop. Regular body check helps preventing bowel cancer. However, not every patient of bowel cancer shows the above symptoms, especially those in early stage.
| Stool test | |
| This is a test which can carry out at home with instruction followed. It detects if there is any hemoglobin presents in stools, so even tiny amount of blood in stool can be found. | |
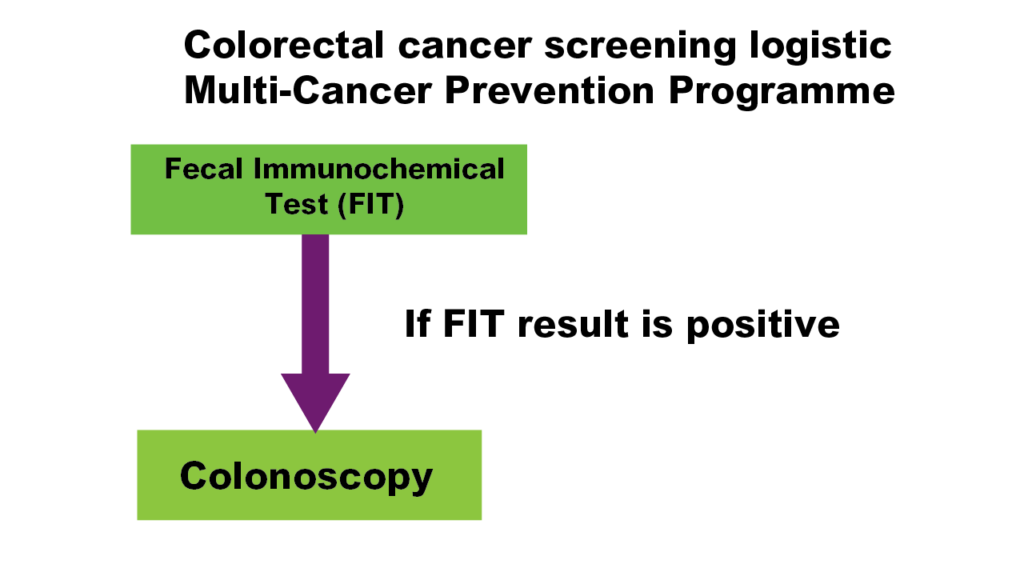
| There are 2 kinds of tests, Guaiac-based Fecal Occult Blood Test, gFOBT and Fecal Immunochemical Test, FIT. FIT is newer than gFOBT. When compared to gFOBT, FIT requires less stool specimen and no diet restriction is needed before testing. Furthermore, FIT is more accurate than gFOBT. | |
| Accuracy: ★★★☆☆ Risk: ☆☆☆☆☆ Fee: ★☆☆☆☆ |
|
| Screening recommendation*: Repeat annually if the result is negative; it should proceed to colonoscopy if the result is positive. | |
|
|
|
| Endoscopy | |
| Flexible Sigmoidoscopy | |
| Flexible sigmoidoscope is a scope with a video camera which is about 60m in length, endoscopists use it to examine the mucosal wall of large intestine by inserting it from anus. The range of examination is up to descending colon. Bowel preparation and low residue diet are needed, seduction and pain killer are injected right before examination to reduce patients’ anxiety and any discomfort. Endoscopists can take biopsy for pathology testing and remove any polyps during flexible sigmoidoscopy. |  |
| Accuracy: ★★★★☆ Risk: ★★☆☆☆ Fee: ★★★☆☆ |
|
| Screening recommendation*: Repeat every 5 years if the result is negative. | |
| Colonoscopy | |
| Colonoscopy is similar to sigmoidoscopy, but a colonoscope is about 1.6m in length, so it can examine the whole large intestine. Bowel preparation and low residue diet are needed. Seduction and pain killer are injected right before examination to reduce patients’ anxiety and any discomfort. Endoscopists can take biopsy for pathology testing and remove any polyps during colonoscopy. |  |
| Accuracy: ★★★★★ Risk: ★★☆☆☆ Fee: ★★★★☆ |
|
| Screening recommendation*: Repeat every 5 years if the result is negative. | |
|
|
|
| Double Contrast Barium Enema, DCBE | |
| Bowel preparation and low residue diet are needed. Enema is needed right before examination. Air and barium solution are injected into large intestine via anus. After that, a series of X-ray films are taken to examine any abnormality. Biopsy taking and polypectomy cannot be done during procedure. |  |
| Accuracy: ★★★★☆ Risk: ★☆☆☆☆ Fee: ★★★☆☆ |
|
| Screening recommendation*: Repeat every 5 years if the result is negative; it should proceed to colonoscopy if 1 or more >6mm polyps are found. | |
| Computed Tomography Colonography, CTC | |
| Bowel preparation and intake of oral contrast is needed. CTC use a special medical instrument to capture a series of pictures of transverse section of bowels, and then 3-dimensional figures are drawn by computer to examine any abnormality. Biopsy taking and polypectomy cannot be done during procedure. | |
| Accuracy: ★★★★★ Risk: ★☆☆☆☆ Fee: ★★★★★ |
|
| Screening recommendation*: Repeat every 5 years if the result is negative; it should proceed to colonoscopy if 1 or more >6mm polyps are found. | |
|
|
|
| *All screening recommendations are based on a joint guideline on screening of colorectal cancer and adenomatous polyps by Dr. Bernard Levin on Gastroenterology in 2008. | |
| Staging | Definition | 5 Year Survival Rate* |
| I | The carcinoma is limited to the bowel submucosa or muscle | 91% |
| II | The carcinoma grows through the bowel wall into pericolic or perirectal tissue, may attach to contiguous organs, but does not invade the lymphatic systems or distant organs | |
| III | The carcinoma invades l or more lymph nodes | 70% |
| IV | The carcinoma metastasize to distant organs (lung or liver usually) | 11% |
* Data extracted from Cancer Statistics, 2010 on A Cancer Journal for Clinicians published by Dr. A. Jemal on 2010
| The data in table on page no. 7 of “Learning About Bowel Cancer” brochure should be as above. The 5-year survival rate of stage II bowel cancer patients should be 91% instead of 70%. |
| According to several medical journals and National Comprehensive Cancer Network, treatment plan of colorectal cancer can be drafted as below. | ||||||||||
|
||||||||||
|
|
||||||||||
| Surgery | ||||||||||
| Depends on patients’ conditions, pre-operative Computed Tomography (CT) scan, Positron emission tomography (PET) scan or ultrasound scan will be carried out to check if there is any metastases and staging of cancer. | ||||||||||
| There are many operation methods, include total colectomy, left/right hemi-colectomy, sigmoid colectomy, etc. by open or laparoscopic resection and they depends on type, size and location of tumors and patient’s condition. The principle of surgery is resection of cancerous part of large intestine or/and metastasized lymph nodes and organs. The 2 cutting ends are then joined up to construct an anastomosis. It is sometimes necessary to open a temporary stoma for defecation so as to help wound healing at anastomosis. The stoma can be removed a few months later through reoperation. Some patients may need a permanent stoma. | ||||||||||
| Endoscopic Submucosal Dissection, ESD |
||||||||||
| Other than open and laparoscopic resections, surgery can be carry out under endoscopy. Endoscopic submucosal dissection provides en-bloc (1 piece) resection of tumor in-situ (stage 0 CRC), those located at submucosa or invaded not more than 1/3 depth of submucosa, and the submucosa underneath. | ||||||||||
| Compared to endoscopic mucosal resection (EMR), ESD can resect a larger leison (>2cm) and resect it in 1 piece with lower recurrence. However, this procedure takes longer time and has relatively higher risk when performed by inexperienced endoscopists. | ||||||||||
| Chemotherapy |
||||||||||
| Chemotherapy uses drugs to interrupt the DNA replication of cancer cells, so as to kill cancer cells. Common drugs used for chemotherapy in colorectal cancer includes Fluorouracil (5-FU®), Oxaliplatin (Eloxatin®), Irinoteca (Campto®), Capecitabine (Xeloda®). | ||||||||||
| Different drugs have different adverse effects, common adverse effects by chemotherapy are fatigue, nausea, vomiting, diarrhea, abdominal pain, anorexia, loss of hair and peripheral edema and redness, etc. To minimize the discomfort caused by adverse effects, patients need to have sufficient rest, balanced diets, increase physical activity, drink more water and quit smoking. | ||||||||||
| Target Therapy |
||||||||||
| Target therapy is different from traditional chemotherapy that it only acts on cancer cells, other normal cells will not be affected, thus, adverse effects of target therapy is less than chemotherapy. Bevacizumab (Avastin®) is a common drug for target therapy. It is an angiogenesis inhibitor which inhibits the growth of new blood vessels and therefore cuts off the blood supply to cancer cells, stop their growth and metastases. Medical researches show that it effectively extends survival though it cannot destroy cancer cells. Common adverse effects are hypertension, fatigue and diarrhea, etc. Severe but rare complication includes gastrointestinal (GI) perforation and internal bleeding. If GI perforation occurs, Bevacizumab needs to stop permanently. | ||||||||||
| Radiotherapy |
||||||||||
| Radiotherapy uses high energy radiation to kill malignant tumors and inhibit benign tumors growth. Clinically, radiotherapy will be fractionated depending on patients’ condition so as to reduce damages on normal cells. Adverse effects caused by radiotherapy include diarrhea, skin inflammation and bowel or bladder bleeding, etc. |
Medical experts believe that lifestyle changing and diet modification can help prevent colorectal cancer. World Cancer Research Fund and National Cancer Institute published a report named ‘’Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective’’ in 2007. This is the largest study of its kinds and the most current and comprehensive analysis of literature on diet, physical activity and cancer.
- Be as lean as possible within the normal range of body weight
- Limit intake of redmeat (beef, lamb and pork) and avoid processed meat
- Eat mostly foods of plant origin
- Be physically active every day in any way for 30 minutes or more
- Limit alcoholic drinks
- No Smoking
And we also recommend
- Have colorectal screening routinely